A progress note turns out to be a vital document to determine the existing condition of the patient, past history, and diagnosis and interventions planned at the moment.
Various health professionals use progress notes to plan further interventions or set up group therapies or even fix goals accordingly.
In this article, a wide range of progress note templates is provided along with the option for nurses, physicians, volunteers, and mental health professionals to update it accordingly based on observations.
Progress note templates Download
1. Medical progress notes – DOC
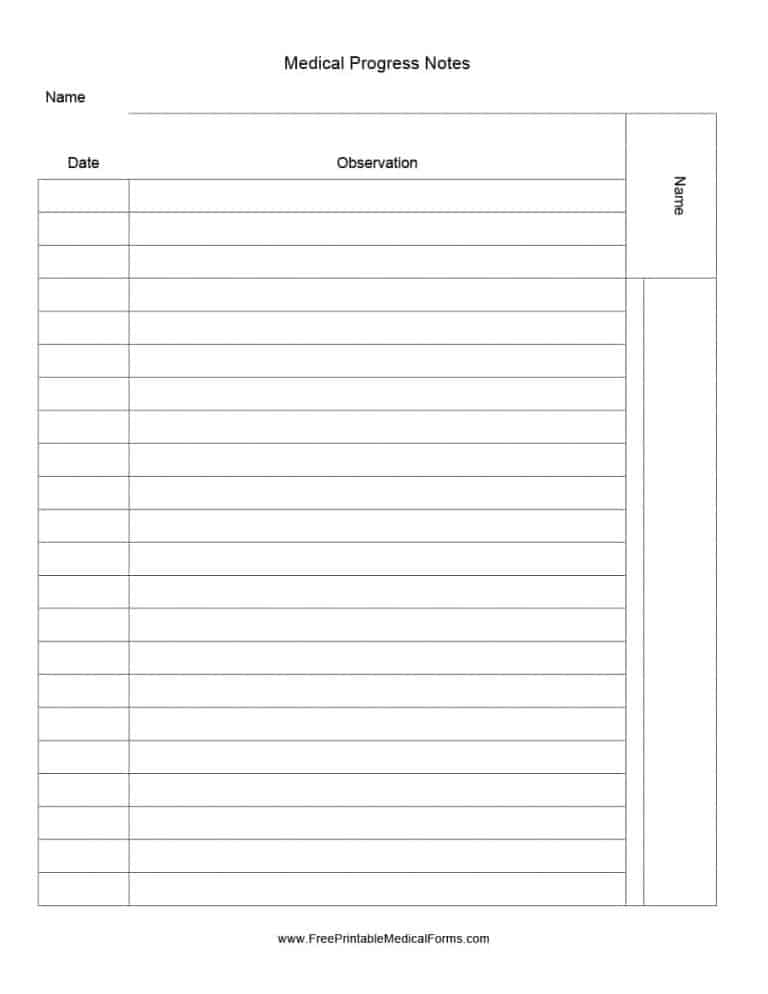
The easiest way to create and maintain a progress note is right in this template. In just three columns, a dedicated record including the progress of the patient is present and all that you will have to do is update as and when you visit the patient.
This can be handy for nurses as well as the physician in planning the intervention going forward.
2. Progress note form DOC
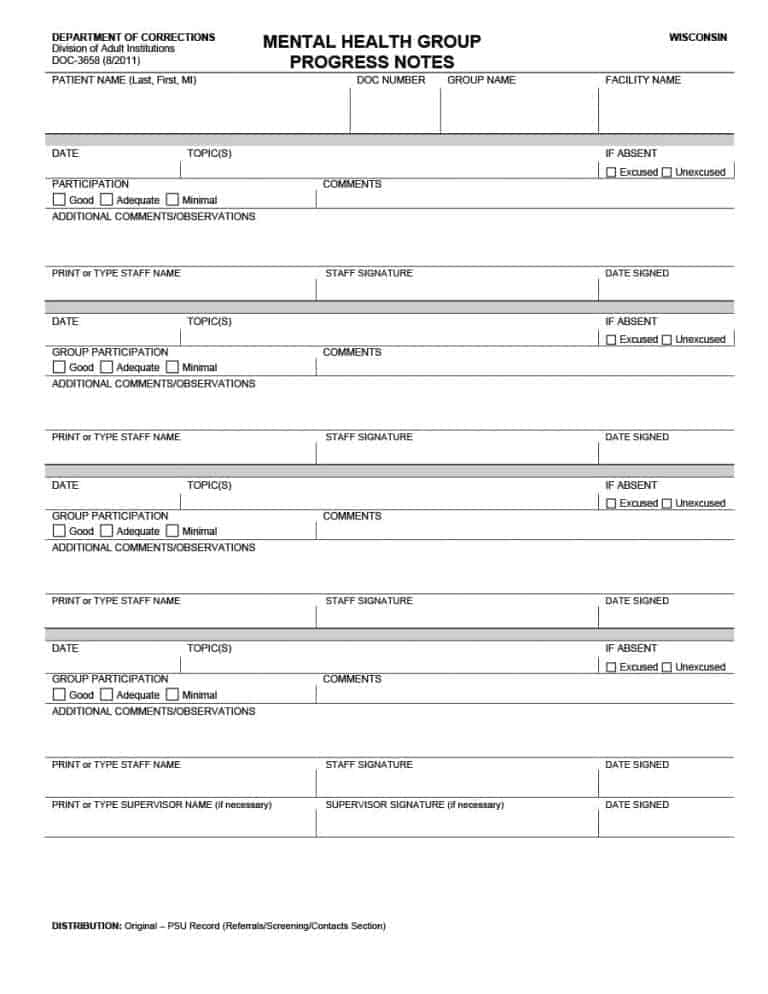
When you handle a patient with a mental health problem, there might be a need for the participation of the group member during counseling.
While progress notes are simple and handy, some experts prefer using a form and update it without having to write in detail. Looking at this template, you have basic placeholders for patient information, the topic covered, key observations, group presence, and signature.
This approach is sufficient if you may have to maintain a record exclusively for the attendance of the patient to the counseling session.
3. Psychotherapy progress note DOC
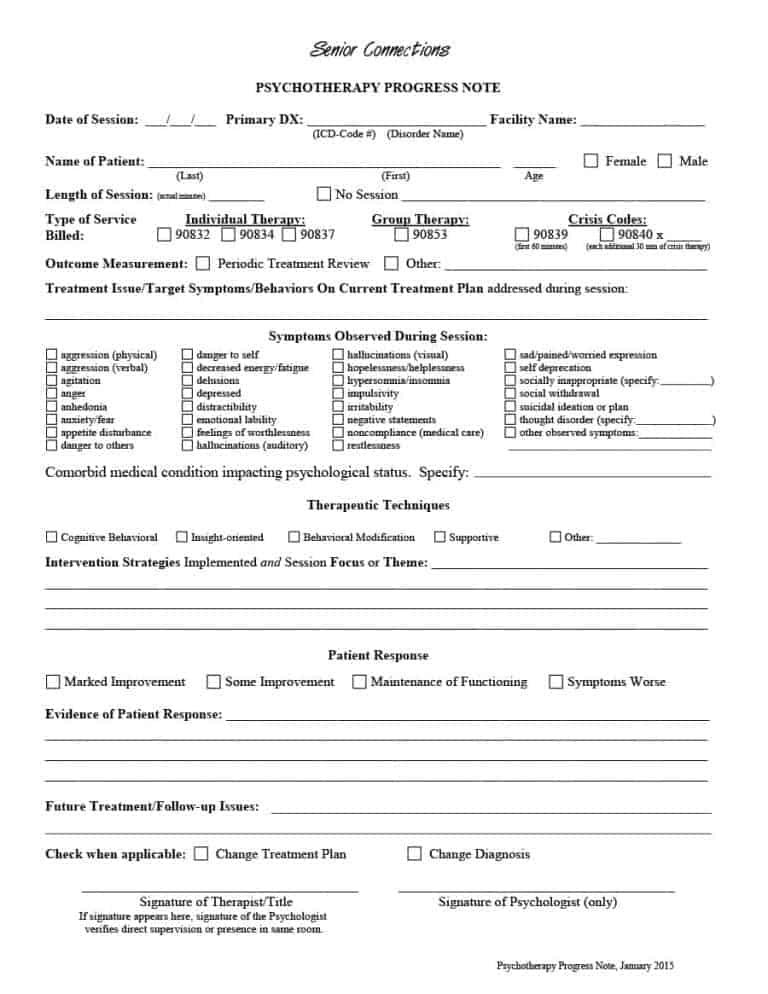
Here is a highly accurate psychotherapy progress note that you can immediately start using for your clients. It includes a format that gets in as much information as possible to update records and also plan interventions accordingly.
For instance, it gathers a detail of the type of service obtained, symptoms, techniques, the response of the client, and the follow-up regimen.
The best part is that this template can be forwarded for the use of a psychologist or any other professionals that have decided to offer supportive service.
4. One-page progress note template DOC
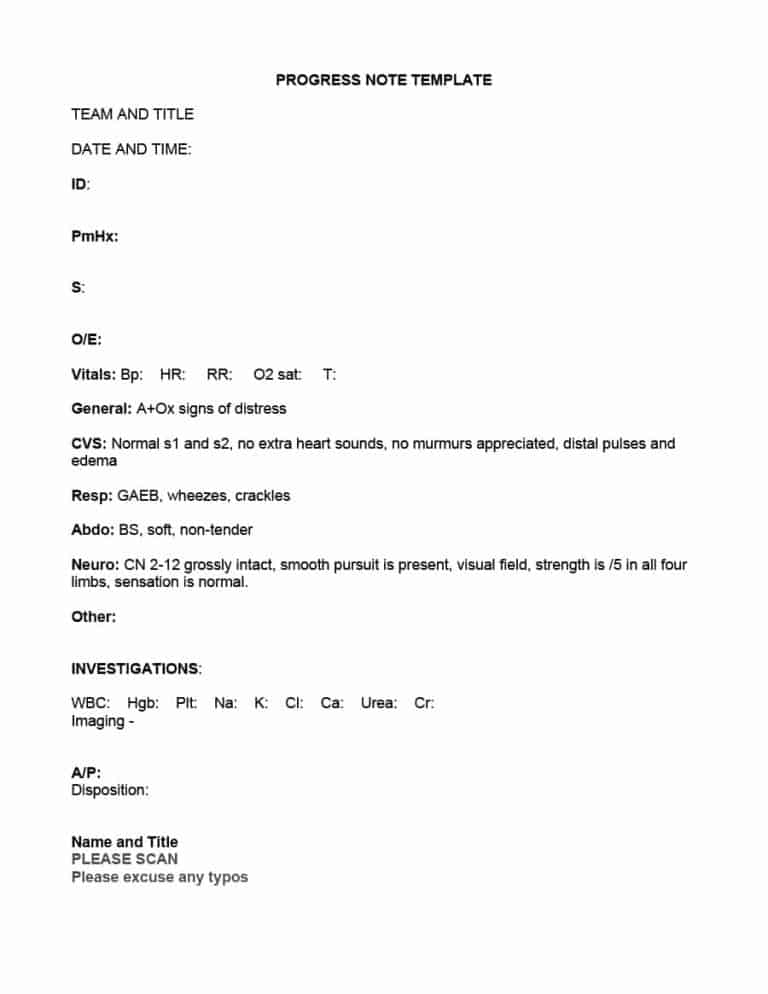
It is habitual for professionals to keep progress notes crisp for the reason that they consult several patients on the same day and it is draining to detail each time.
The purpose of this one-page template is to input sufficient information in a brief way including vitals, abdomen, respiratory functioning, WBC, imaging, disposition, and any other suggestions to meet the health need.
If you have a clinic, it is a better idea to append the logo, header, and footer about your organization.
5. Counseling progress note DOC
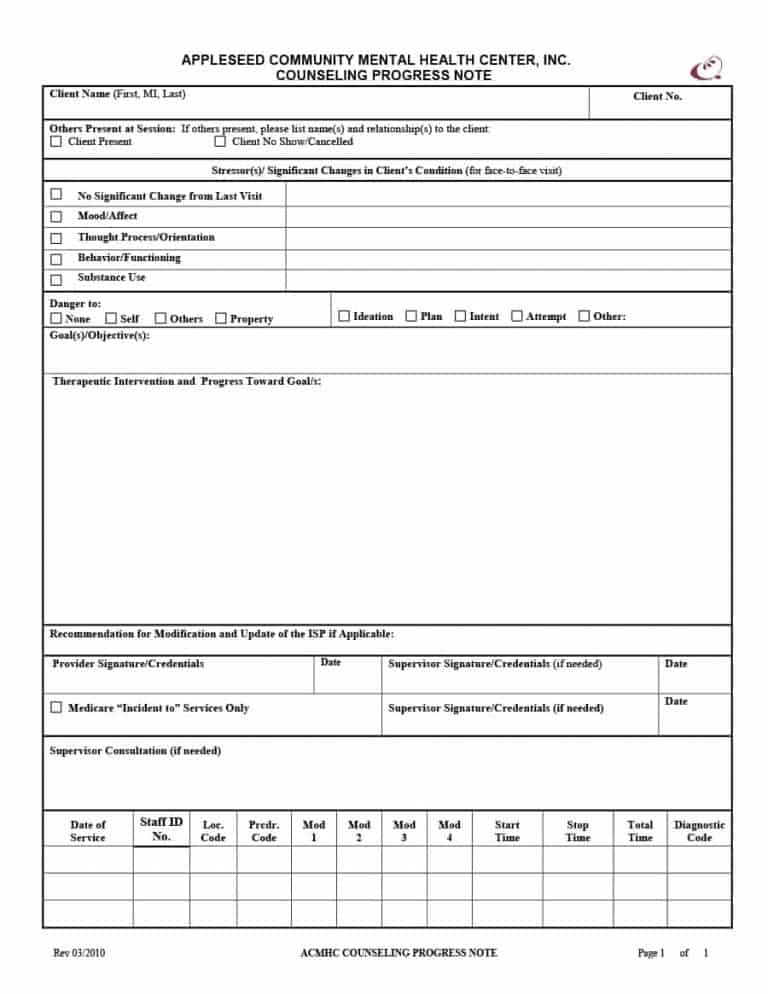
The success of any treatment lies in how well the patient is responding to the current treatment approach.
When it comes to psychological counseling, it is mandatory for patients to revisit the specialist at regular cycles until better health is observed.
The aforementioned template gathers information related to improvements seen, therapeutic intervention decided, consultation of any other supervisor, and the duration of the counseling.
6. SOAP progress note DOC
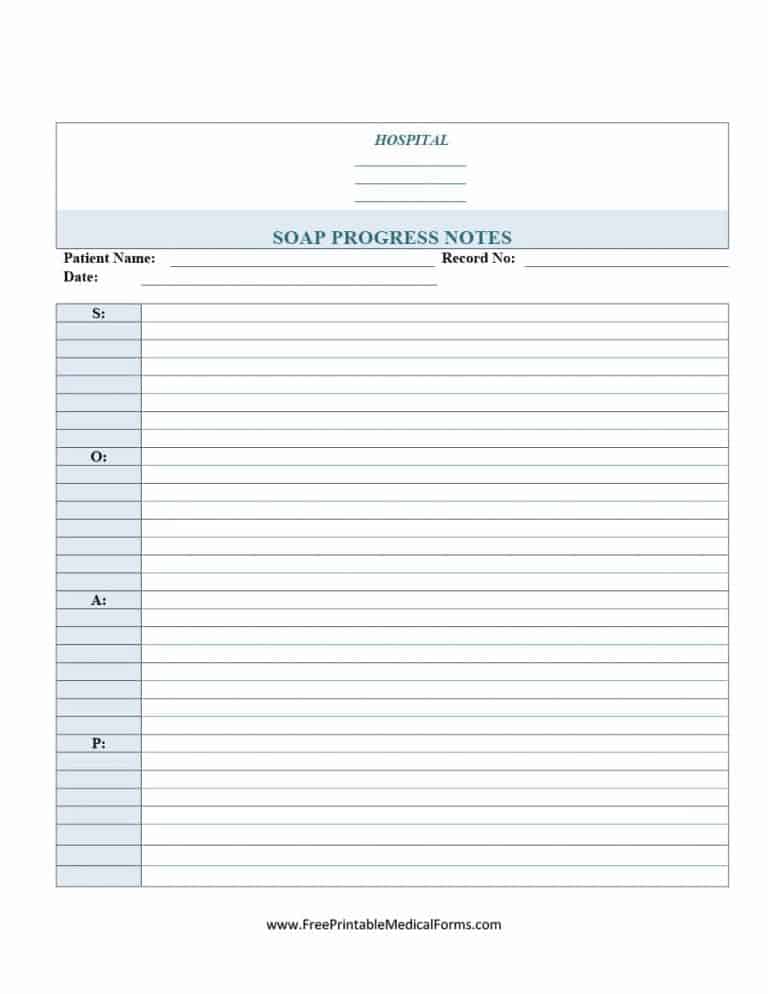
SOAP stands for subjective, objective, assessment, and plan. It is commonly used by nurses and therapists mainly to update information about the patient based on observations. This is by far the standardized approach followed by nurses to keep an eye on how the patient has responded so far.
There are two things that you can do with this template.
- One is to categorize the identifications and also note down the respective professional that can help towards the intervention.
- Another approach is to divide it into multiple columns and also maintain a checklist so that the nurse does not have to input detail each time. Instead, the nurse can simply tick those problems that persist.
7. PATH Progress notes DOC
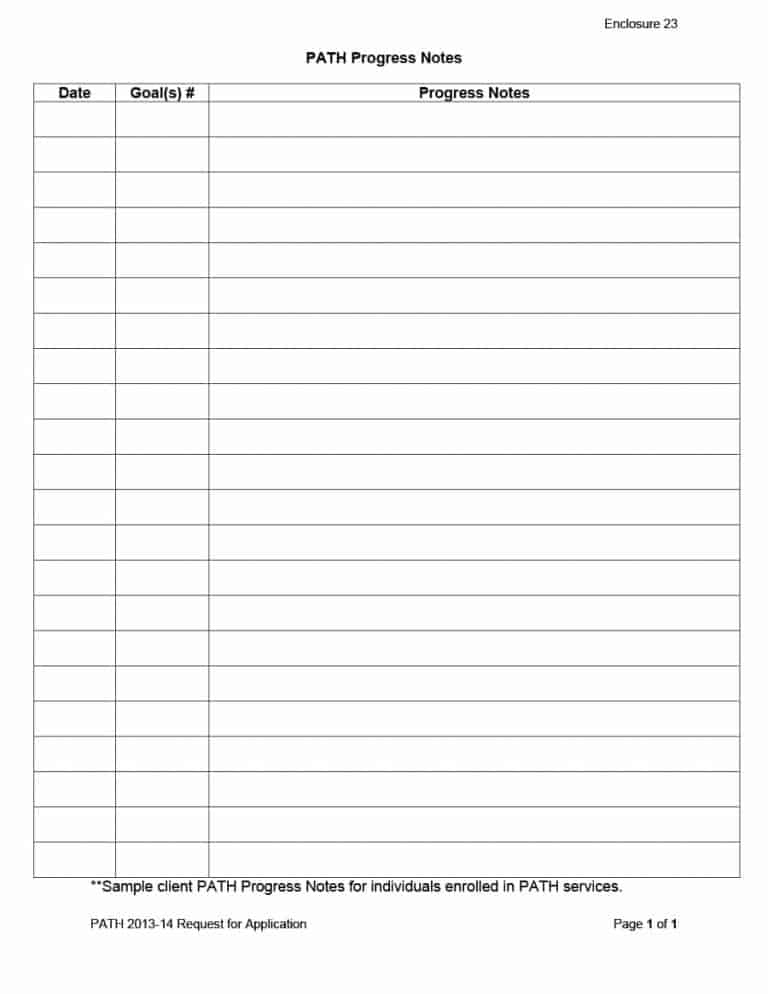
Progress notes are used for a specific reason and it is essential for health experts to understand and acknowledge the reasons before they put such notes to use.
Path certified progress note follows an approach that guides other professionals to offer services as per the PATH framework.
It is as simple as it could be. For instance, it includes columns for dates, goals, and progress notes. However, every goal that is mentioned gives the insight to the therapist to offer the service accordingly and also as per the PATH framework.
8. Pictorial patient progress note DOC
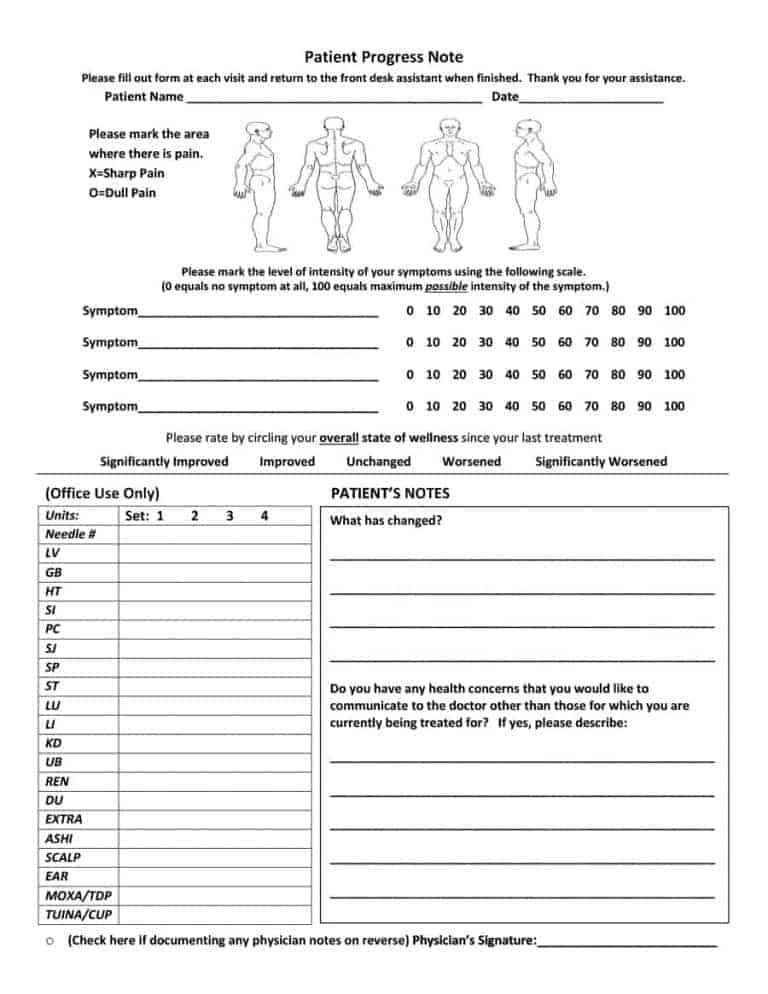
The most interesting part of this template is its pictorial representation which gives a quick idea of pain symptoms and interventions.
As soon as they are marked, there are also two sections for the patient and the service provider to enter necessary inputs that can add more value to the treatment.
It is going to be an integrated approach where multiple people involved in the treatment share their views and ideas about the concept.
When patients write down notes related to experiences and treatment, it indicates the impact level of the treatment and this also influences the satisfaction score of the patient towards treatment. On the other hand, the nurse/administrator can append any other data related to patient management.
9. Volunteer progress note DOC
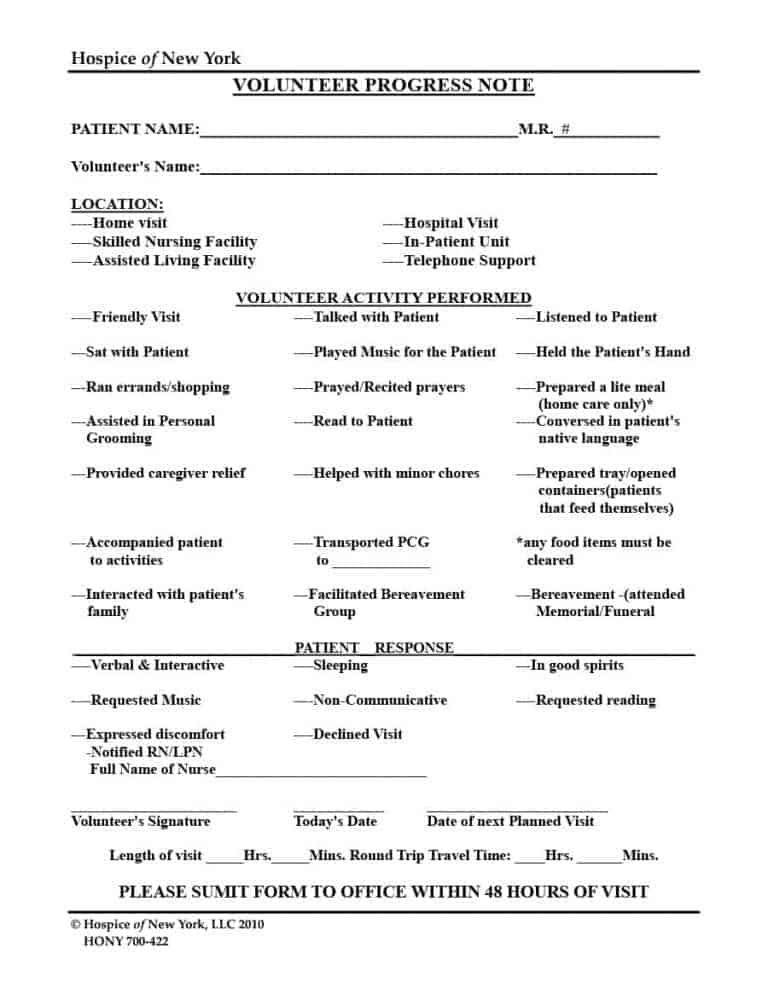
Progress notes are not just meant for therapists and patients. Volunteers also play integral parts in counseling and treating a patient till the stage of recovery. This template is designed exclusively to enable volunteers to enter observations in respective fields based on the visit or interaction with the patient.
This template can be used by public agencies or any non-profit organizations that have several volunteers to follow up with the patient and provide support towards treatment. This is probably the case even during the case of COVID-19.
Now that you have several progress note templates to choose from, it is time to get it right by knowing certain points about it.
Frequently asked questions
1. How do you write a progress note?
When you write a progress note, you may have to maintain legibility and also explain the entry as well as an intervention approach. The best bet is to avoid manual errors as much as possible. While they do happen, getting it supervised by another expert would reduce error and improve the worthiness of the note.
Also, when you write a progress note, you may have to eliminate unnecessary blank spaces and make it as crisp as possible because it helps in simplifying things.
2. What to include in a progress note entry?
While writing a progress note entry, it is mandatory to ensure well-written language and update about the observation. Also, conciseness, relevance, and objectiveness are a few areas that should be adhered to. These help in giving a clear perception of facts.
3. Are progress notes and SOAP notes the same?
Perhaps! The SOAP note is a type of progress note meant to append particular information about the patient in a format enabling the reader (patient or his/her family) to gather a grip of every element associated with the session.
The only difference is that a SOAP note comes in the same format and cannot be changed since it belongs to a standard. On the other hand, a progress note can fall into a wide range of formats as well as detailing.
4. Who can use a progress note?
In the healthcare scenario, anyone from nurses to physicians to volunteers can use it. Before using it, it is essential to ensure that the person holds the appropriate authority to gain access to the patient’s detail and dive into other aspects relating to the health of the patient.
The person should also know how to use it. This is because inappropriate information or idea about the subject can end up in negative consequences and dissolve the purpose of a progress note.
5. Are there any legal requirements related to progress notes?
When you use templates for filling in progress notes for patients, you must be aware of the legal framework and regulations associated with patient confidentiality, safety, treatment protocols, and information gathering.
In any instance, the progress note might be accessed at a later stage and hence, details related to outcomes, action plan, reassessment, risks, and changes will have to be updated as and when appropriate.
Conclusion
It is the responsibility of a physician or a nurse to update the progress note immediately upon consulting the patient. Several templates mentioned in this article can be of extreme use in understanding the interventions, approaches followed by the therapist, and also in improving recordkeeping capability. It eliminates the mess related to managing records.
Before you use it, remember to go through the laws of your state!


